When doctors at the Lumbini Provincial Hospital in Butwal heard from the hospital administrators that Tzu Chi Foundation, an international Buddhist charity headquartered in Taiwan, was donating two ventilators to the regional health facility in June 2020, they were elated. For the last three months, one of the biggest hospitals of southwestern Nepal had been serving thousands of Covid-19 patients with just four ventilators existing in the hospital for several years. And, the aid from the foundation would prove crucial for the critical cases they had been receiving every day.
As planned, representatives of the Department of Health Services under the central government handed over the aid to the hospital’s driver Khem Dhungana in Butwal on June 23.
But, as Dhungana delivered the supplies to the hospital administration, something unexpected happened. When biomedical engineers Prem Raj Basyal and Joban Shah opened the boxes, there were no ventilators in them. Instead, the boxes contained two BiPap machines, devices that help patients facing difficulties in natural breathing.
The engineers immediately realised the department had not checked what were inside the cartons while dispatching them to the hospital. “We informed the concerned officials about the delivery and we chose not to use the BiPap machines,” Basyal says. He adds the hospital did not require additional BiPap machines as it already had a sufficient number of such machines. An administrative official at the hospital reveals the engineers had also raised concerns over the quality assurance procedure in front of the team.
This is just the tip of the iceberg. An Onlinekhabar investigation reports that Nepal’s public health bureaucrats do not bother to scrutinise medical equipment, including ventilators, received from international donors as grant support for the Covid-19 response in terms of quality assurance, putting patients’ lives at the mercy of these unchecked machines.
Donor-dependence
The government of Nepal was more underprepared for the Covid-19 pandemic than most other governments in the world given its under-resourced public health system. Most hospitals in the country were operating in the absence of critical equipment, compelling the government to depend on foreign governments and charities for support as soon as the pandemic struck the country in March 2020.
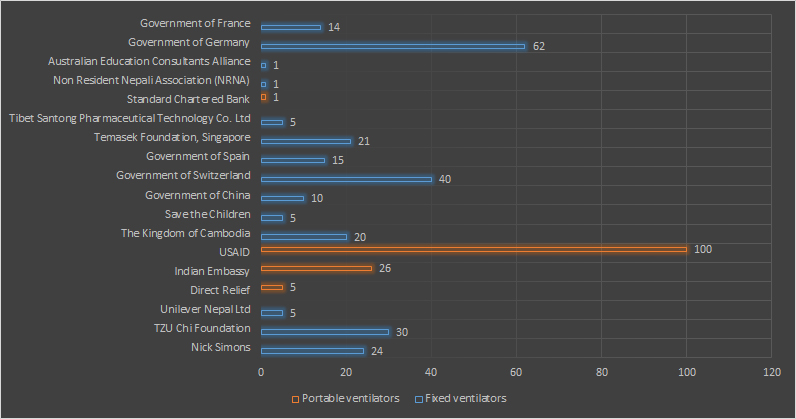
The most apparent form of dependency was about the management and distribution of ventilators. From March 2020 to June 2021, Nepal received at least 253 (fixed) ventilators and 132 portable ventilators from different international donors, informs the Department of Health Services. Despite some media reports claiming the government purchased a few ventilators in the period, the department has no record of buying any such machine on behalf of the central government although provincial governments have bought some.
Moreover, federal health officials do not have concrete answers on why they did not procure any. Dr Dipendra Raman Singh, chief of the department under the Ministry of Health and Population, passes the buck on Dr Bhim Singh Tinkari, the director of the department’s Management Division. Meanwhile, Tinkari refused to respond to Onlinekhabar’s repeated questions on the issue.
Ventilators that have been donated are brought to Nepal via road and air routes after which the Ministry of Health and Population takes charge of the machines. The ministry assigns the department to keep a record of the machines before delivering them to the health centres. In many cases, the donors themselves specify where they want the machines to be installed whereas the department decides where to keep the other machines.
The aid has been crucial for the government to combat the crisis. For example, before the pandemic broke out, the Karnali province had only four ventilators. But, last year, the provincial government purchased 12 more ventilators to combat the Covid-19 crisis whereas various donors provided 18 more on a grant, directly and via the federal government, taking the total number of ventilators to 34, informs Provincial Health Director Rabin Khadka.
The neighbouring Sudurpaschim province was also reeling under the crisis with only four ventilators in operation before the pandemic. Provincial Health Director Guna Raj Awasthi says the provincial government bought 20 ventilators after the virus was detected in the province. The province’s Health Equipment Supplies Management Centre’s Public Health Inspector Laxmi Kumar Shrestha says the provincial government also received seven other ventilators from various donors directly and over a dozen via the federal government as a grant.
It means the donors’ contribution was as significant as the government’s investment in some cases whereas, in others, it was even more.
The donors’ involvement made the addition of new machines to the country’s public health system much easier than the government buying them as the public procurement procedure would have taken a longer time than receiving donations, further aggravating the situation, says Dr Bishal Dhakal, who founded a ventilator charity campaign Nepal Ventilator Services to help hospitals access the machines as required during the pandemic.
Check-marking sans checking
The government found an easy route by depending on the donors rather than going through the lengthy process of procurement that entails a lot of red tape. However, it was not able to ensure the machines received met the quality standards required for the critical care of patients. Officials themselves acknowledge the lapses.
It was only after the Butwal Hospital informed of receiving the ‘wrong’ machines that officials of the Department of Health Services under the central government learned about the crucial error in the system. “The foundation that supplied the equipment said they were ventilators and we supplied accordingly,” a senior staffer at the department’s Management Division says. “We did not open the box to verify the machines that had been received on a grant.”
Mukunda Bista, the foundation’s representative involved in some recent conversations with the government, also confirms the BiPap machines were first thought to be ventilators. “Yes, we were wrong in understanding them as ventilators; they were some other machines,” Bista, who introduces himself as a senior volunteer of the charity, says, suggesting it should not be an issue now as the government records have already been corrected.
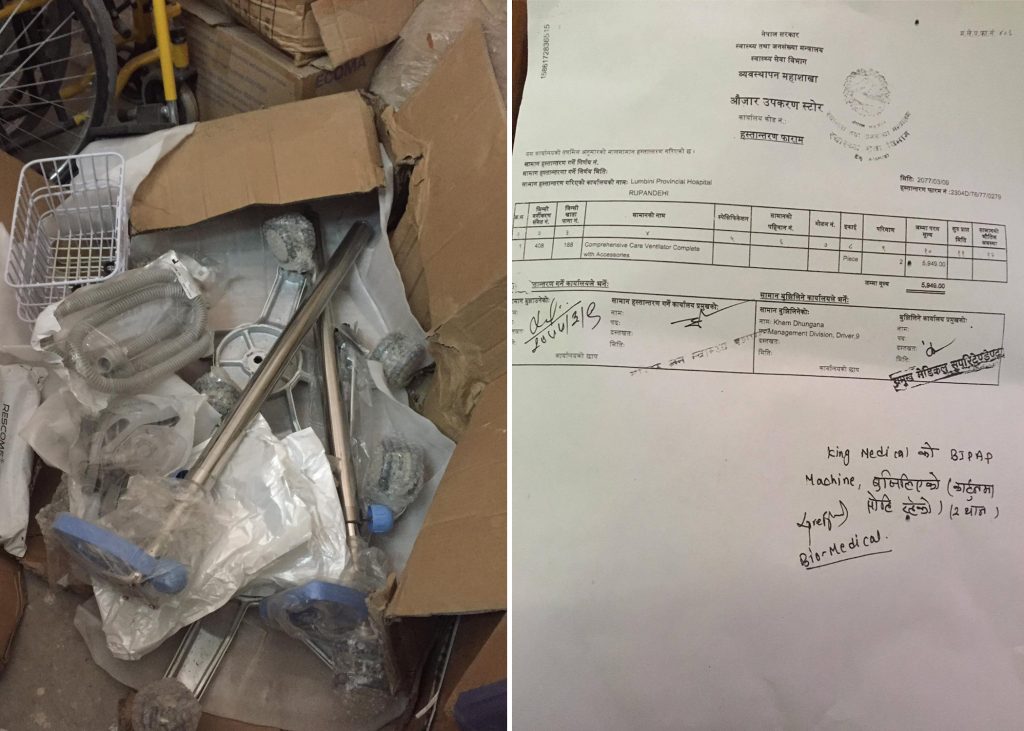
Bista does not have any substantial answer on why the foundation mistook BiPap machines for ventilators even though there are apparent differences. Their sizes and shapes are distinct as well as the price; a BiPap machine costs around Rs 500,000, but a ventilator is worth at least Rs 2 million.
Bista instead points at the lack of the foundation’s concrete organisational setup and workforce in Kathmandu for the misunderstanding. He says the foundation’s headquarters directly sends supplies to Kathmandu, sometimes from China and at other times from Malaysia, and the job of the foundation’s ‘volunteers’ here is just to facilitate the handover and report it to the headquarters.
The organisation has not been registered with the country’s INGO regulator, Social Welfare Council, and hence is free from any government scrutiny applicable to NGOs and INGOs in the country. Bista says the registration is not necessary because the organisation does not have an office in Nepal. “Our involvement is rather personal here.” On his part, the council’s spokesperson Durga Prasad Bhattarai says the council cannot take any action in such cases. He says the government itself has to investigate such issues.
That particular incident, however, impelled the Department of Health Services to change its system. It began verifying whether the machines were as specified by the donors and checking their physical condition before dispatching them to the field. Nonetheless, this is the only task the department carries out in terms of quality assurance as far as non-purchased equipment is concerned. “It is because if there were any serious faults in the equipment, we could not return them,” says the staffer on a condition of anonymity.
Policy-practice gaps
However, Dr Bikash Devkota, who was the chief of the Quality Standards and Regulation Division of the Ministry of Health and Population in June 2020, claims the government could return any machine received as a grant if it was found defective. But again, he hastily mentions that is moreover a moral responsibility of the donor to avoid defects — a clear suggestion that the government’s hands are tied. “If the documents forwarded by any organisation and the machines that have been donated do not match, it is the responsibility of the concerned organisation,” he states.
Dr Devkota, who led the ministry’s Quality Standards and Regulation Division until April 2021, claims the government approves donations only after it verifies the goods are useful. “The equipment is received only after we know their specifications. We research about them on websites of the manufacturers and other sources before approving the donation.”
Meanwhile, Dr Devkota’s successor Dr Madan Kumar Upadhyaya was unavailable for comments.

However, the BiPap machines that are gathering dust at the Butwal Hospital because they were dispatched without any quality assessment are evident of several gaps that exist between policies that Dr Devkota talks about and the practices in the field. Officials in the Department of Health Services who coordinate medical supplies for all government health facilities across the country also agree with this.
Padma Mishra, a biomedical engineer at the department, says the engineers sometimes get to know about the equipment only after they arrive in the store. For example, another biomedical engineer closely following the issue says that most of the 100 ventilators that USAID donated to the government on November 13, 2020, were sent to different hospitals directly from the Tribhuvan International Airport in Kathmandu itself.
Hence, when it comes to donations it is only occasionally that the engineers can recommend specifications and check the equipment against the set criteria. Mishra reveals she was able to specify the criteria of the machines being received on aid only once in the past few months. “We had decided each technical requirement of the ABG and ultrasound machines provided by JICA, but recently, a lot of machines have arrived and I do not know what they are.”
Many machines gathering dust
There is another incident that contradicts the ministry’s claim about scrutinising the quality of equipment delivered. Dr Bikash Devkota, as the chief of the Quality Standards and Regulation Division of the Ministry of Health and Population, had told Onlinekhabar in January 2021 that around four per cent of the medical equipment and medicines purchased and received through aid during the past year for the country’s Covid-19 response is stored in the ministry’s warehouse as they cannot be utilised due to various reasons. The government has not been able to make the suppliers take back the unused goods for which it has spent millions of rupees, let alone those received for free.
There are similar examples at the hospital level also. In the previous year, over 10 hospitals in Bagmati province received medical equipment from China. Among them, the Bhaktapur Hospital received six ICU units and three ventilators.
“All three ventilators could not be used as they also required oxygen plants to operate,” says the hospital’s Medical Superintendent Dr Sumitra Gautam.

Meanwhile, the doctors detected some serious errors in the machines. “The biomedical engineers had checked the machines for oxygen leakage problems and found them satisfactory. But, when a patient was shifted to a ventilator, it showed errors with dropped saturation levels, forcing us to shift the patient to another ventilator immediately.”
Thus, in the absence of alternative ventilators, emergencies such as these could have serious health implications, fears Dr Gautam.
A biomedical engineer who has closely observed the functioning of these ventilators for research purposes says many of the ventilators donated to Nepal’s health facilities last year did not function when required. “All it takes is a single trial to notice that the equipment does not supply oxygen in severe cases like when a Covid-19 patient is intubated,” the engineer says.
“If this is the scenario with a hospital that boasts of one of the finest medical services and human resources, I don’t think the donated ventilators that are installed at other hospitals in the provinces are functioning,” Dr Gautam says.
Meanwhile, the Chinese Embassy in Kathmandu says it does not know anything about such issues as it has not monitored the functioning of the donated equipment. In response to a list of questions about the problems, the embassy’s Media Liaison Officer Luan Xiutan told Onlinekhabar that the embassy did not have the information that was sought. “They are quite technical. Please understand.”
Inadequate workforce
The aforementioned cases concern just around four per cent of the equipment remaining unused. The remaining 96 per cent of the machines and medicines, most of which are unchecked in terms of quality assurance because they were received free of cost, are thus being used to test and treat patients across the country. Even at some big hospitals, there is no mechanism or official to check if the equipment is functioning properly.

For example, the Narayani Sub-regional Hospital in Birgunj, a city in southern Nepal that borders India, has been in operation without a biomedical engineer. As Birgunj was one of the first Covid-19 hotspots in Nepal in early 2020, the presence of biomedical engineers could have been very helpful, says the hospital’s Covid-19 in-charge Dr Udaya Narayan Singh.
Dr Singh says it is the doctors there who check if the machines including ventilators are working properly. “We don’t have engineers. Neither do we have any mechanism to technically judge if the machines are okay. If we (doctors) detect any problem while reading the statistics on the monitor, we will call engineers from other places,” he adds.
Meanwhile, the Jaleshwar Hospital in Mahottari of Province 2 also has a similar story. The hospital has five ventilators, but none of them is in operation effectively. The hospital neither has doctors qualified to operate the machines nor sufficient biomedical engineers capable of checking their quality regularly, says the hospital’s emergency in-charge Sakesh Karn. “Had we been equipped with enough medical staff, half of the Covid-19 patients in emergency cases could have been treated promptly,” he says.
There are several such stories across the country.
The assistant spokesperson for the Ministry of Health and Population, Dr Sameer Kumar Adhikari says the country currently has over 2,000 ventilators including those received as a grant from foreign governments and agencies. He says the ministry does not have any data on how many of them are operational but accepts the number of non-operational ventilators and those requiring maintenance is significant.
The government of Nepal has not created any permanent position for biomedical engineers in the country’s public health system yet, neither does it seem to care much about their presence. “All of these engineers currently working at our hospitals are appointed on the contract basis,” informs Upendra Dhungana, the chief of the Supplies Section in the Department of Health Services, who is in frequent contact with hospitals across the country. “Moreover, we do not know how many of them are still employed.”
Shyam Sundar Haluwai, the president of the Nepal Biomedical Association, an organisation of biomedical engineers across the country, says his association has been advocating for the inclusion of biomedical engineers in the country’s health system, but the government has always turned a deaf ear. “Perhaps, there is more to gain in not checking and repairing the machines so that they can purchase new ones frequently, thus receiving heavy commissions in the process,” he laments.
Dr Dipendra Raman Singh, the chief of the Department of Health Services, acknowledges this gap and admits their role could be important in the country’s health system. He, nonetheless, assures that the ministry is revising its organisation and management (ONM) plan, which will establish some permanent positions of biomedical engineers at major government hospitals across the country.
Rana Bahadur Gharti Magar, the chief of the Logistics Management Information Resource Centre in the department, informs some donors themselves have taken the initiative to fill this gap. According to him, the donors can mobilise their engineers on the site for installation and maintenance purposes if they feel the need. For example, USAID deployed some of them for the installation of 100 ventilators at different hospitals in Nepal. Over the past year, the government received at least 285 other ventilators from several donors and they have been sent to different health facilities across the country, but instances of the donors deploying engineers on their own are only a few.
Important post-installation examinations ignored
While there are no skilled human resources to properly install ventilators at the hospitals, it is apparent that any mechanical fault that appears during their operation goes unchecked for want of a capable workforce. This discrepancy is taking a toll on the patients’ health directly.
Dr Bishal Dhakal of Nepal Ventilator Services says regular checks and maintenance of the machines are a must to ensure they work properly. “If there is no regular maintenance, almost 50 per cent of the machines become defunct over time,” he informs.
Dr Dhakal assumes the donors must have provided quality equipment, but there could be faults at times and adds it has been impossible for the government of Nepal to thoroughly scrutinise the equipment received as aid due to the emergency. When the country’s health bureaucrats are not qualified to even keep proper records of the received and distributed machines with their proper specifications, expecting them to check each part and function of the machines regularly before and during the use does not sound practical, he states.
Nonetheless, in such cases, biomedical engineers at respective hospitals can help the government ensure the quality of the donated machines, a biomedical engineer working for a Kathmandu-based government hospital says. “Checking the machines after the installation is as important as the quality assurance before installation because sometimes the functions do change automatically,” the engineer who wishes to be unnamed says. “We were shocked to discover that some ventilators were supplying around 300 ml of oxygen only when the monitors displayed 500 ml.”
According to him, such faults are likely with the purchased machines also, but those received on aid are more liable as they undergo a poor quality assurance checking. As the central officials are likely to dispatch the goods even without unboxing them as revealed in the case of the Butwal Hospital, post-installation checking becomes more important, according to him.
A senior medical officer at the Shahid Gangalal National Heart Centre in Kathmandu agrees with the engineer that post-installation scrutiny would be more important for the equipment received for free. Leave ventilators aside, even small donations such as PPEs might have quality issues when they are donated, according to him. “We had rejected some PPEs when we found out that their quality was compromised,” he says, “Quality check and overall assessment of the equipment before and during its use is mandatory. It has to be even more meticulous when they come from donors or external sources.”
Way forward
For this to happen, there should be sufficient human resources first, according to experts. Dr Rakshya Pandey, a senior consultant for pulmonary and critical care medicine at the HAMS Hospital, says ensuring the availability of skilled human resources to operate the ventilators is as important as making such machines available to a hospital. For her, this is just one part of the bigger problem of the country’s public healthcare system, which the pandemic has revealed.
“Not every doctor can operate a ventilator,” she says, “If people operating this machine are not skilled, the ventilators may cause unwanted disadvantages because only severely critical patients who have difficulties in breathing need ventilators and many things need to be looked at. ”
But, apparently, there are no skilled human resources to check and operate these machines. The consequence is that doctors have felt ventilators have not been as effective as expected in terms of the treatment of Covid-19 patients in Nepal. But, the Health Ministry says it has not received any complaints about mechanical defects in the machines received during the crisis.
Nonetheless, medical professionals tell Onlinekhabar that the pandemic — including complaints about the lack of quality assurance checking and reports of the inefficiency of such machines — has given the government and other stakeholders a chance to delve into the vulnerabilities of the country’s health system. They view this should be considered a lesson to improve the system and be prepared for such disasters in the future.
“Definitely, this experience would have been different if we had groomed our health system in the first place,” says a senior medical officer at the Gangalal Hospital in Kathmandu. “Quality check is an important component, but it is still questionable whether the nation has a reliable system and mechanism to track these discrepancies.” He thinks it is the health workers’ responsibility, primarily, to find the faults and make suggestions to correct them.
Although beggars cannot be choosers, the Department of Health Services, which has the sole authority over the donated medical equipment, should strictly maintain the quality assessment and need-based distribution system, says Dr Dhakal. “This is the maximum we can do as we cannot decide on what equipment we would like to receive as a donation.” In addition, the government should make its public procurement policy more transparent and should also make public all the information about the donations received, according to him.
Meanwhile, Dr Pandey observes the way the government has been receiving medical equipment from international donors and distributing and using them has ignored established standards and regulations, hence, reforms should begin at the government’s level. “There is an absolute failure in the system’s functioning. The laws should be strongly implemented and the government should play its part by being more accountable.”
“This is the time to reflect on our mistakes, learn from our experiences and train our workforce accordingly.”
(In collaboration with Onlinekhabar.com. Top Raj Sharma in Butwal and Suresh Bidari in Birgunj also contributed reporting.)